Problem
The ICU at the Brooklyn Hospital Center faced overwhelming challenges with severe staff and resource shortages, forcing nurses to perform triage under immense pressure. Overstretched frontline workers couldn’t provide individualized care, often leaving patients unsupervised following a risky ‘first-come, first-serve’ approach. This was extremely problematic in high-stakes life-or-death situations leading to significant risks in life-or-death scenarios.
Solution
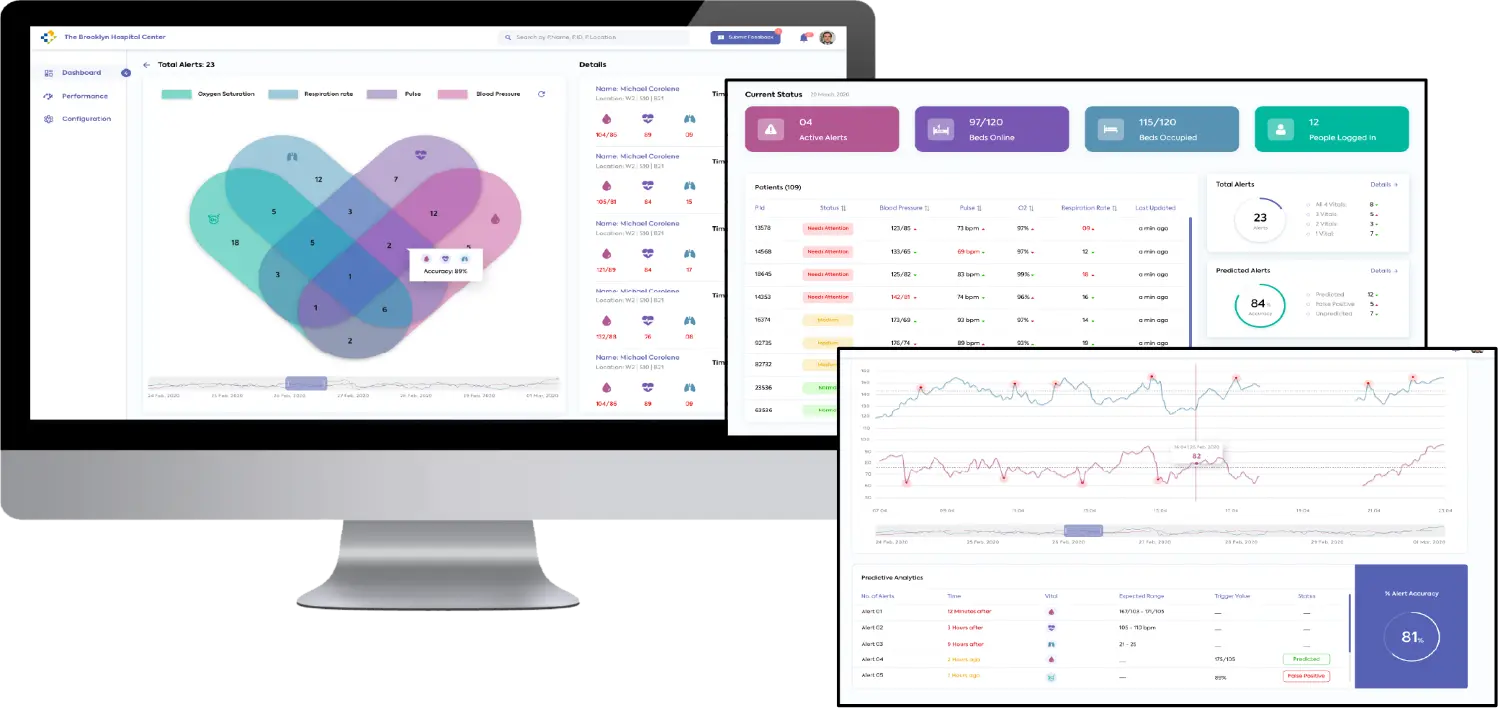
Techolution developed an AI model that analyzed ICU data, including blood pressure, heart rate, body temperature, and oxygen levels, to prioritize patient care. The medical staff was alerted for patients at higher risk of life-threatening episodes (“coding”), learning from patient data patterns to predict and prevent critical conditions.
Impact
Techolution’s AI model enabled efficient resource allocation, improved patient outcomes, and helped nurses prioritize critical patients, saving more lives with optimized effort. Tested during the first wave, the model was ready for deployment during the second wave, meeting an urgent need in the crisis.
As the COVID-19 pandemic swept across the United States in early 2020, New York City found itself at the epicenter of the crisis. The city faced unimaginable devastation, with over 21,000 lives lost in just three months. The overflowing morgues, refrigerated trucks holding dead bodies and constantly ringing ambulance sirens were proof of how grim the situation was.
Hospitals were stretched to their limits, with healthcare workers facing grueling hours and acute shortage of protective equipment. Not to mention the exponentially growing threat of the deadly virus.
Answering New York City’s Call For Help
Although New Yorkers cheered for healthcare workers every day, banging their pots, pans, and playing instruments, they needed more than just appreciation. They required resources to effectively respond to the crisis. Brooklyn Hospital Center had previously sought Techolution’s help to transform their data infrastructure with AI. However, now faced with the misery of the pandemic they were eager for help. Although initially unsure, they let us help their frontline workers fight the outbreak.
Before Techoultion stepped in, the ICU at the Brooklyn Hospital Center faced overwhelming challenges. Nurses, working round the clock, struggled to provide individualized care to every patient amidst severe shortages of staff and resources. Their intensive care unit (ICU) was overwhelmed, forcing medical staff to perform triage to decide which patients qualified for beds and who received limited medical supplies, among many other impossible choices.
Many patients were dying every single day, with sick people queuing up outside the doors waiting to be seen. In the short-staffed ICUs, nurses focused on moving quickly between patients, unable to give each one the much needed individual attention. They would check each person periodically, but had to leave them unsupervised most of the time. Initially, they would circulate through every patient in a “first-come first-serve” order, which seems fair when you are handing out ice cream or chocolates, but can be problematic in such high stakes life-or-death scenarios.
Saving Lives With AI-Powered Patient Prioritization
So how did Techolution solve this problem using AI, even before ChatGPT brought artificial intelligence into the mainstream? We started by using data from ICU monitors, like blood pressure, heart rate, body temperature, and oxygen levels. We built an AI model that used ICU data to determine patients' risk of death and leveraged this information to alert medical staff on whom to prioritize for urgent attention with the help of our LLM. This model learned from changing patient data over time to predict who was at higher risk of “coding.” In this context “Coding” is a medical jargon for having a life or death episode.
This implementation enabled more efficient allocation of resources and improved patient outcomes. Moreover, by anticipating these events, the AI we built could notify nurses which patients to prioritize, helping them save more lives while optimizing their workload. We built and tested the AI based patient prioritization model during the first wave of the virus which helped us deliver an effective solution that was ready to be deployed in the field once the second wave hit. This allowed us to meet an urgent need in a time of crisis.